How to improve urgent referrals? The power of collaboration and a service design approach
This project produced fascinating insights and shone a light on the power of collaboration to enhance and improve this life-changing service
With recent events resulting in the NHS being pushed to breaking point, the stakes have never been higher for a service that so many of us rely on. Having prioritised responding to the COVID-19 pandemic, NHS Trusts across the UK now have a backlog of referrals which have been delayed or escalated over the past 18 months.
York and Scarborough Teaching Hospitals NHS Foundation Trust saw that it was about time to focus on how the urgent referral service is currently working and explore how it might be improved.
So, the Trust appointed dxw and CCD, a human-centred design agency, to discover how referrals requesting urgent and emergency care result in patients receiving the right care, in the right place, at the right time.
This project not only produced some fascinating insights but shone a light on the power of collaboration to enhance and improve this life-changing service.
The goals of the project, while a challenge, were:
- to map the Trust’s current urgent referrals service, including what works well, and any problems and pain points
- to envision a future service including recommendations, concept designs, and prototypes for the highest value improvement ideas
A unique partnership
Although CCD and dxw have previous experience working in healthcare, this project was a unique experience for both companies as it focused more on clinical decision making.
Together, with our team of Trust stakeholders, we had to consider the tense, pressurised decision making processes that are unique to urgent care. We also drilled down into some of the culture of the Trust and explored the collaboration blockers which can arise, both across primary and secondary care, as well as within the hospitals themselves.
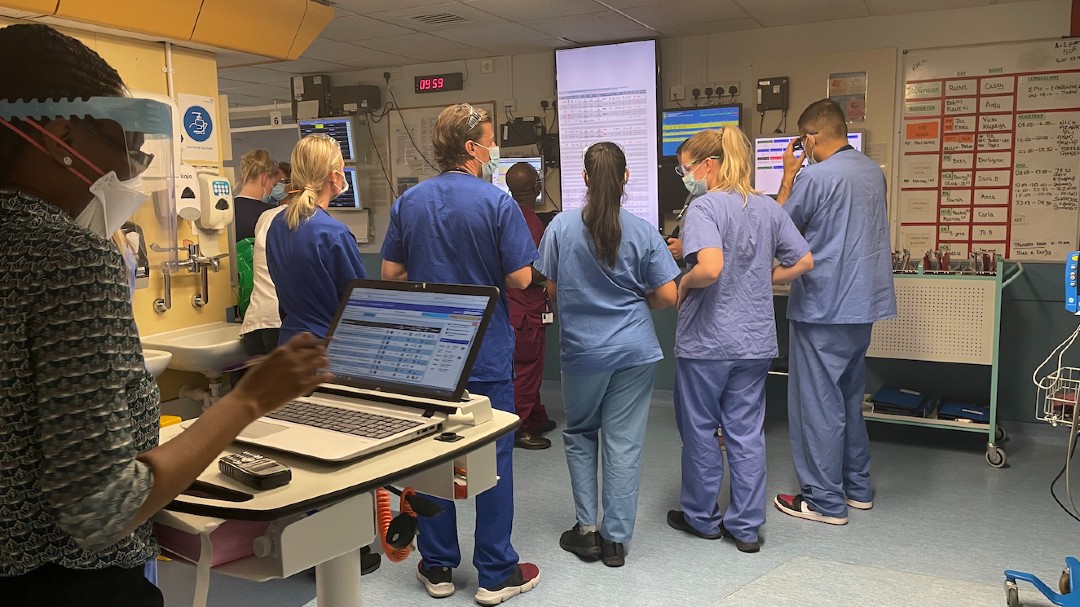
Our partnership had to respond to the mixed physical and digital needs of the project. This was unusual, as dxw primarily works with the digital aspect of services while CCD have more involvement with the built environment and physical, on-the-ground experience. Working to our strengths, we took a mixed team of CCD and dxw representatives on a site visit to both Scarborough and York hospitals. This was invaluable to our understanding of the problem area and influenced the proposed solutions but it also helped us uncover and truly understand the human impact and physical and emotional stressors that flow through the process.
dxw and CCD used a user-centered service design approach, incorporating a design sprint to learn and meet the goals of this discovery project. While this was a first for the Trust, and an area they were keen to be a part of and learn from, both dxw and CCD are well versed in adapting these methodologies to meet the needs of projects.
We felt humbled by working with medical experts and the cooperative way in which they treated the project alongside their patient duties, as well as carefully and clearly explaining the reasons behind care and medical decisions.
The challenge: availability and time
With hindsight, the timeline was quite tight and made more challenging due to the complexity of the broad and loosely defined area of urgent referrals.
There was a core team from the Trust, including clinical leads and nurses as well as representatives from digital and information teams, who attended most of the project meetings like planning sessions, standups, and show and tells. However, due to the demanding nature of their work, it was difficult on occasions to get everyone together at the same time.
We overcame this by being flexible in our methods and approach and being open in our communications, sharing our progress, and plans with all members of the core Trust team. We held regular drop-in standups for those of the Trust core team who were available to keep them updated. By adapting the sprint to meet the needs of the project and the limitations of time/availability of the team, we made sure we had as many of the Trust team contributing as possible.
Defining urgent referrals
It became clear quite early on that there are many varying definitions of what urgent referrals are, why they exist, and what happens when patients get referred there. It was challenging enough to understand it to be able to then analyse it and make recommendations.
We decided to make the challenge of defining “urgent referrals” a central part of our interviews with clinical and administrative staff across the Trust asking, “How did each department and each individual think of urgent referrals?”
During user research, we were frequently directed by interviewees to other people and groups who could add to our understanding of urgent referrals. The challenge here was knowing when to stop. If time and resource permitted, we would have explored as many leads as possible, however with the already limited project timeline, the team had to conduct live gap analysis and prioritisation tasks to agree what areas were a must-have-now and which were more appropriate for a future stage of research. For those on the team we were unable to meet with, we generated a full and detailed list of other parties and representatives that the Trust should engage with to continue this area of work.
The scope of the project
Another component of the project was how to align the areas we were looking into, across all of the urgent referral pathways and the Trust itself, to other ongoing or developing areas of work happening at hospital level, Trust level, and the wider NHS.
We were anticipating this to be a challenge, however we weren’t prepared for how difficult it would be to identify these workstreams in the first instance. With so many departments working with their own funding streams and no direct point of contact who oversees these projects. We now recognise how this initial obstacle was actually a real opportunity for improvement.
Learning to transform referrals
What was overwhelmingly clear from the outset is that no one challenge with the referrals process is ever isolated. Each area, department, or opportunity within the Trust will impact another. Many pathways and processes in a single Trust are interwoven from years of delivery and incremental evolution. We learned that you can never just focus on “urgent referrals” because the nature of it impacts Accident & Emergency, Diagnostics, bed management, and discharge. They’re all interdependent and interlinked.
We learned that all departments feel pressure to care for patients and discharge them as soon as possible. This pressure can get passed on from one department to another and can cause conflict, while the varying ward discharge processes add additional complexity.
There are tangible opportunities to improve referrals but it needs buy-in from all parties, including executive teams and budget holders. In addition, technical integration into existing digital infrastructure and reducing steps and handoffs need to be central to any potential solutions for them to be adopted.
The Trust is open to the use of service design and more will need to be done to continue to use design thinking and service design approaches, to go beyond the discovery phase and actually really integrate a solution – not just add another one. This would need buy-in from across the Trust and all those who’ll be using it. It’s evident that the capacity for the necessary level of engagement in a service design process is not necessarily available due to the massive operational pressures.
This was a genuine and successful partnership delivery between dxw and CCD and the Trust who we’re currently in talks to address how they deliver on the recommendations.